If you’ve ever worn a continuous glucose monitor (CGM) without having diabetes, you know the feeling: you eat breakfast, your line rises, and suddenly you’re wondering if that peak means something is wrong. Add in sleep, workouts, stress, and caffeine, and your “normal” can start to feel like a mystery.
Here’s the calming truth: a normal glucose range on a CGM is less about one perfect number and more about patterns, including where you sit overnight, how high you rise after meals, and how quickly you come back down.
CGMs also don’t measure blood glucose directly. They estimate glucose in interstitial fluid (the fluid between cells), so readings can lag behind a fingerstick by several minutes, especially when glucose is changing fast. In this guide, you’ll learn realistic CGM ranges for most non-diabetics, how to read your trends without spiraling, and when it’s smart to follow up with labs.
What “normal glucose range” looks like on a CGM for most non-diabetics
When people say “normal blood sugar levels,” they often mean lab values. In a clinic, fasting glucose normal is commonly described as about 70 to 99 mg/dL. CGM data usually looks a bit messier because it’s continuous, it captures real life, and it includes sensor noise.
The goal isn’t to keep your glucose flat like a tabletop. A healthy body is supposed to respond to food, activity, and hormones. Think of glucose like a tide: it rises after a meal, then returns toward shore.
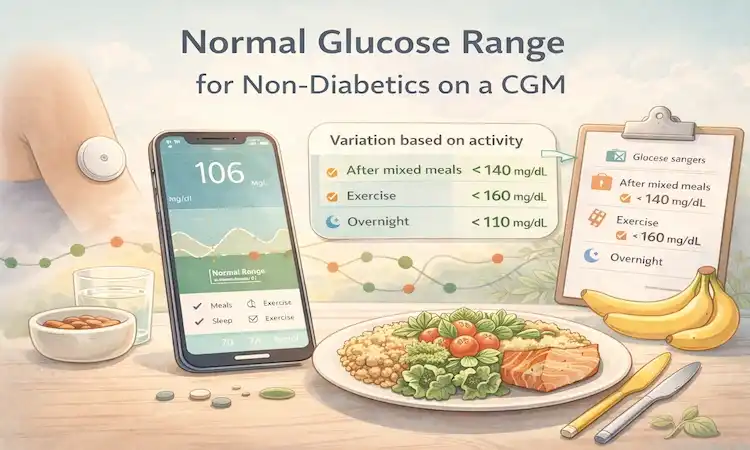
Many healthy adults tend to see a daily CGM pattern like this (numbers vary by person, meal, and sensor):
- Overnight band: often roughly 70 to 90 mg/dL, with some people drifting into the high 60s during deeper sleep.
- Pre-meal range: commonly around 75 to 95 mg/dL (sometimes higher in the morning).
- Post-meal peak range: many meals peak under about 140 mg/dL, and plenty of people peak lower depending on what they ate.
- Time to settle: glucose often trends back toward pre-meal levels within about 2 to 3 hours.
If that list makes you think, “Mine doesn’t look like that every day,” you’re not alone. A CGM captures stress spikes, rushed lunches, poor sleep, and workouts that labs never see. Research that tracked CGM in healthy adults also shows there’s a real spread in what “normal” looks like day to day, even without diabetes, as described in this multicenter CGM study in healthy participants.
Fasting, overnight, and between meals: the baseline numbers to know
“Fasting” usually means no calories for 8 to 12 hours, so your morning reading (before food or coffee with cream and sugar) is the closest everyday proxy.
On a CGM, a steady overnight line often sits in a relatively narrow band. If you see small waves, that’s normal. Your liver releases glucose overnight, and hormones shift as you cycle through sleep stages.
Some healthy people briefly dip into the high 60s while asleep. If you feel fine and it’s short-lived, it may be your normal. If you wake up sweaty, shaky, confused, or hungry and the CGM shows lows, that’s different, confirm with a fingerstick and talk with a clinician.
Morning numbers can run higher for reasons that have nothing to do with “bad metabolism.” A late dinner, alcohol, dehydration, poor sleep, and even a rough night with snoring can nudge your morning glucose up. Your body is trying to keep you fueled, not punish you.
After you eat: a realistic postprandial glucose range and peak timing
“Postprandial” just means after eating. On a CGM, glucose often rises within minutes of starting a meal, with a glucose peak after meals commonly showing up around 30 to 90 minutes later (timing varies). Because of sensor lag, the peak may appear later than what’s happening in your blood.
A practical postprandial glucose range for non-diabetics often includes peaks below about 140 mg/dL for many meals, followed by a steady drop. What matters most is the curve, not a single high point.
Meal makeup changes the curve a lot:
- A bowl of refined cereal on its own can create a sharp hill.
- The same carbs paired with eggs, Greek yogurt, nuts, or fiber-rich fruit often makes a gentler slope.
- Fat and protein can slow digestion, shifting the peak later and sometimes making it last longer, even if it’s not as tall.
If you want a science-based view of everyday CGM curves in healthy people under real-life conditions, this paper on continuous glucose profiles in healthy subjects is a helpful reference.
How to read your CGM patterns without overreacting
A CGM can be a mirror, and mirrors can mess with your head if you stare too long. One odd day isn’t a diagnosis. One weird spike after a restaurant meal doesn’t mean you’re “becoming diabetic.” Your job is to zoom out.
Instead of hunting for a single perfect number, focus on a few simple trend checks:
- Are you spending most of the day in a reasonable band for a non-diabetic?
- Do your meals create manageable rises that don’t linger?
- Does your overnight line look fairly steady most nights?
Also remember that many CGM apps estimate things like “GMI,” which is meant to approximate A1C. It can be interesting, but it’s not the same as a lab A1C for everyone, especially in people without diabetes.
If you’re using a CGM for wellness (not diabetes management), it helps to treat it like a learning tool. Some companies now market CGMs directly to non-diabetics, which has fueled curiosity and confusion. For context on this trend, see CGM for people without diabetes.
The 5 CGM clues that matter most for non-diabetics
Here are five ways to interpret your day without getting lost in tiny fluctuations:
- Most of the day in a healthy band: Look for “mostly steady” rather than “perfect.” Occasional bumps are normal.
- Peaks that aren’t too high and don’t last: A brief rise after meals is expected. Long plateaus up high are more meaningful than short peaks.
- A smooth-ish overnight line: Big overnight swings can reflect late meals, alcohol, poor sleep, or sensor issues.
- Fewer large swings: The size of your ups and downs matters. A roller coaster day often tracks with skipped meals, high-sugar drinks, or high stress.
- How you feel during dips: Numbers matter, but symptoms matter too. If you feel shaky, weak, or confused, treat that seriously and confirm.
If you want a clear definition of “postprandial” and why it matters, this overview of postprandial blood sugar lays out the basics in plain language.
Common “false alarms” on CGM (and what to do instead)
CGMs are useful, not flawless. Some alerts and weird readings are just tech problems or timing issues.
Common false alarms include sensor lag (especially after exercise or fast carbs), “compression lows” when you sleep on the sensor, and noisier readings on the first day of a new sensor. Hot showers, dehydration, and loose adhesive can also distort readings.
When something looks extreme, use a simple rule: if it doesn’t match how you feel, verify before you panic. Wash your hands and confirm with a fingerstick, especially for suspected lows. Then log what was happening, food, stress, exercise, sleep, and see if the pattern repeats over several days.
If you want a quick reference for typical non-diabetic targets as described by a CGM maker (note that this page uses mmol/L and mg/dL), see Dexcom’s explanation of normal blood glucose levels.
Why your “normal” might look different: age, hormones, exercise, and food choices
Two healthy people can eat the same meal and see different CGM curves. That doesn’t mean one is broken. It means biology is personal.
Age can change insulin response over time. Sleep quality changes hormones that regulate appetite and glucose. Menstrual cycles can shift glucose sensitivity week to week. And if you’re in a calorie deficit, training hard, or under stress, your liver may release more glucose to keep you going.
Food matters too, but not in a moral way. Some meals simply digest fast. A banana eaten alone can hit differently than a banana eaten with peanut butter. Liquid carbs can spike more than the same carbs in solid form.
Context is the missing piece. A slightly higher morning number might be your body’s normal “wake up” signal. A workout spike might be your muscles calling for fuel.
Morning rises, stress spikes, and workout bumps that are still normal
Many people see higher readings in the early morning due to the “dawn effect,” a normal rise in hormones like cortisol that helps you wake up. Stress can do something similar. A tense meeting, poor sleep, pain, or illness can push glucose up even if you didn’t eat.
Caffeine can add to this in some people, especially on an empty stomach. If your morning coffee seems to raise glucose, try testing it with food versus without food, or after a short walk.
Exercise adds another twist. Steady cardio often lowers glucose during or after the session. Short, intense work (sprints, heavy lifting) can raise glucose first because your body releases stored fuel. Later in the day, you may see improved stability as muscles refill glycogen.
Hydration and recovery matter. If you’re under-fueled, under-slept, or dehydrated, your curve can look choppier.
Meals that create big spikes, and simple ways to smooth the curve
Big spikes often come from fast carbs with little fiber or protein, especially in liquid form. Sugary coffee drinks, juice, soda, candy, pastries, and a bowl of white rice or pasta eaten alone are common examples.
If you want a smoother curve, you don’t need extreme rules. Small tweaks can change the shape of the wave:
Add protein or fiber to carbs (chicken, beans, yogurt, nuts, veggies). Start meals with salad or vegetables when you can. Take a 10 to 15-minute walk after eating. Watch portion size with refined carbs. Try to avoid grazing late into the evening, which can keep glucose elevated overnight.
The goal is comfort and consistency, not chasing a “flatline” graph.
When to follow up with a clinician, and what tests actually answer the question
A CGM can hint at patterns, but it can’t diagnose diabetes or prediabetes by itself. If your CGM data keeps looking outside expected ranges, or you have symptoms that worry you, a clinician can help you sort signal from noise.
Bring context, not just screenshots. A few days of CGM graphs plus a simple log of meals, sleep, exercise, illness, and stress gives a much clearer picture.
This also matters if you’re planning pregnancy, already pregnant, or have conditions that change glucose patterns (like PCOS), because the thresholds and follow-up steps can differ.
CGM signs that are worth checking out
Consider a medical check-in if you notice repeat patterns like:
- Fasting readings above the typical normal lab range on most mornings
- Post-meal peaks that stay elevated beyond about 3 hours, especially if it happens often
- Low readings with symptoms, confirmed by a fingerstick
- Large, unexplained swings that don’t match food, exercise, or stress
Also be extra cautious if you have a strong family history of diabetes, a history of gestational diabetes, PCOS, or you’re taking steroid medication, all of which can shift glucose.
Helpful labs and what they mean (fasting glucose, A1C, and OGTT)
Three common tests can answer the “is this normal?” question more clearly than a CGM alone:
- Fasting plasma glucose: A lab snapshot after an overnight fast.
- A1C: An average of blood glucose over roughly 2 to 3 months (it’s an estimate, not a perfect mirror of CGM averages).
- Oral glucose tolerance test (OGTT): A structured test that checks how your body handles a glucose drink over time, sometimes used when answers are unclear.
Lab blood draws can differ from CGM because they measure glucose in blood, not interstitial fluid, and because CGM accuracy varies by device and situation. If you’re worried, bring a few days of CGM graphs and your notes so the conversation stays grounded in patterns.
Conclusion: Aim for patterns, not perfection
A normal glucose range for non-diabetics on a CGM usually looks like mostly steady readings overnight and between meals, a reasonable rise after eating, and a return toward baseline within a few hours. Brief spikes happen, and a single strange day doesn’t mean anything by itself.
Give yourself at least 1 to 2 weeks of data before drawing conclusions. Look for repeat trends, and use context like sleep, stress, and exercise. If your CGM patterns are consistently outside what you’d expect, or you have symptoms, get lab tests and talk it through with a clinician.
For a simple next step, run a 3-day test: keep one meal the same, take a 10-minute walk right after, and note how you slept the night before. Your CGM data in your glucose hub will start to make more sense.

Gas S. is a health writer who covers metabolic health, longevity science, and functional physiology. He breaks down research into clear, usable takeaways for long-term health and recovery. His work focuses on how the body works, progress tracking, and changes you can stick with. Every article is reviewed independently for accuracy and readability.
- Medical Disclaimer: This content is for education only. It doesn’t diagnose, treat, or replace medical care from a licensed professional. Read our full Medical Disclaimer here.