Ever had “butterflies” before a big test, then felt your stomach flip like it’s doing gymnastics? Or noticed that one stressful week can change your bathroom schedule fast? That’s not you being dramatic. It’s your body running a tight feedback loop between your head and your gut.
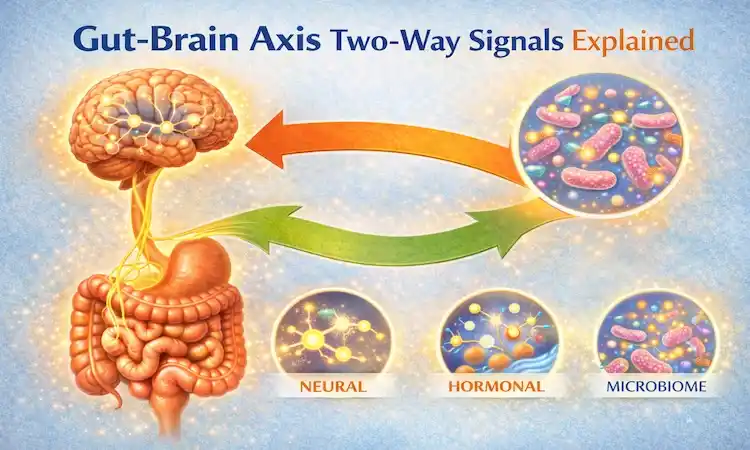
The gut-brain axis is the two-way communication system between your digestive tract and your brain. It runs through nerves, hormones, and immune signals, and it helps explain why emotions can change digestion, and why digestion can shape mood, energy, and focus.
In this guide, you’ll learn what the two-way signals are (in plain English), how stress affects digestion in real time, why gut microbes can change the “message,” and what simple habits can support healthier gut brain communication without extreme rules.
The gut brain axis in plain English, who is sending messages to whom?
Think of your body as a group chat. The brain is not the boss that sends one-way commands. Your gut talks back, all day long. This is the brain gut connection explained in the simplest model: your gut and your brain are two busy centers, and they trade updates constantly.
When the brain sends messages down to the gut, it can change hunger, nausea, cramps, and how fast food moves through you. When the gut sends messages up to the brain, it can shift stress response, sleep, motivation, and even how “loud” pain feels.
That’s why symptoms can show up on either side. You might notice:
- A nervous stomach, nausea, or urgent bathroom trips before a meeting
- Constipation during a stressful month
- Low mood or brain fog after days of poor sleep and off meals
- Appetite changes when anxiety is running the show
Researchers describe this system in detail, but the key idea is simple: it’s a loop, not a straight line. For a deeper science overview of how the gut and brain interact, see The Gut–Brain Axis (Annual Review of Medicine).
Your main communication routes, nerves, hormones, and immune signals
The gut-brain axis pathways are like three main routes your body uses to send updates.
First, there are nerves, including the vagus nerve, a major “phone line” connecting gut and brain. Your gut also has its own nerve network called the enteric nervous system (people call it the “second brain”). It helps run nervous system digestion, including muscle movement that pushes food along, even when you’re not thinking about it.
Second, there are hormones, which act like broadcast messages. Stress hormones like cortisol can change appetite, acid levels, and gut movement. Hormones don’t “talk” in words, but they change body settings fast.
Third, there are immune signals. When your body senses irritation or infection, immune messengers can increase inflammation. That can change how sensitive your gut feels and how your brain responds to stress.
A quick analogy: nerves are like direct texts, hormones are like group notifications, and immune signals are like a system alert that makes everything feel more urgent.
Why your gut bugs matter, the microbiome as a message maker
Your gut is home to trillions of microbes. They don’t just sit there. They break down parts of food you can’t digest on your own, especially fiber, and they produce chemicals your body can use.
One example is short-chain fatty acids (SCFAs), made when microbes ferment certain fibers. SCFAs can support the gut lining and may influence immune activity. Microbes can also affect neurotransmitters. For instance, serotonin is involved in both mood and digestion, and a lot of serotonin-related activity happens in the gut (that doesn’t mean “fixing your gut” automatically fixes depression, it’s more complicated than that). A solid primer on microbiota and mood is The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health.
Your gut lining and its mucus layer work like a smart filter. They help decide what gets through to your bloodstream and what stays in the gut. When the filter is irritated, messages can change.
Daily life shifts these signals more than most people realize. Diet changes, poor sleep, antibiotics, illness, travel, and even a short stretch of high stress can nudge the microbiome and the gut’s barrier, which can change how the brain reads what’s happening below.
From brain to belly, how stress changes digestion in real time
When people say stress affects digestion, they often mean one of two things: stress changes how the gut works, and stress changes how the gut feels.
Your brain’s job is to keep you safe. So if it thinks a threat is near (a deadline, conflict, money worries), it can switch your body into a high-alert mode. That shift is useful if you need to run. It’s not as helpful if you’re trying to eat lunch calmly.
In stress mode, blood flow can shift away from digestion toward muscles. Your gut movement (motility) can speed up or slow down. Acid and enzyme output can change. The gut can also become more sensitive, so normal stretching from gas or food can feel like pain.
Occasional stress is normal. The system is built for it. The problem is long-term stress, when your body stays keyed up for weeks. Then the gut may not get a clean “return to calm” signal, and symptoms can hang around longer than they should.
A 2025 review on stress and gut-brain connections goes deeper here: Stress, microbiota, and the gut–brain axis in mental and digestive health.
What happens during fight or flight, motility, acid, and cramping
Here’s the chain reaction in everyday terms.
Your brain senses a threat, even if it’s just social pressure. Your nervous system shifts into fight or flight. Your gut gets the memo fast.
For some people, the gut speeds up. Food moves faster, water doesn’t get absorbed as well, and stools get looser. That’s why stress can trigger diarrhea or urgency.
For others, the gut slows down. Movement gets sluggish, stools dry out more, and constipation shows up. Some people even swing between both, depending on the type of stress and timing.
Stress can also increase stomach acid for some people, which may worsen burning or nausea. Cramping can happen when gut muscles contract in an uncoordinated way, or when the brain turns up the volume on normal gut activity.
Anxiety gut symptoms, why worry can feel like a stomach problem
Anxiety gut symptoms are common because anxiety changes how your brain scans your body. When you’re worried, your brain looks for danger signals. That makes normal digestion sensations feel bigger and more alarming.
Common anxiety-linked gut sensations include bloating, nausea, stomach pain, early fullness, and appetite changes. Some people get a “tight” throat or a queasy wave that feels like it comes out of nowhere.
It’s still important to know when symptoms need medical attention. Talk to a clinician soon if you have blood in stool, unexplained weight loss, fever, severe or worsening pain, or symptoms that wake you up at night. Those aren’t “just stress” signals, and you deserve a real evaluation.
From gut to brain, how digestion can shape mood, energy, and focus
The loop also runs upward. Your brain constantly monitors the gut for clues about safety, energy supply, and inflammation. If the gut sends “all clear,” the brain is more likely to stay steady. If the gut sends repeated distress signals, the brain may shift into a more defensive state.
One route is inflammation. When immune activity is higher, the brain can interpret that as “something’s off,” which can affect mood and fatigue. Another route is microbial byproducts, including SCFAs and other compounds produced during digestion. These can influence signaling in the body, including nerves and immune pathways.
There’s also the simple issue of nutrient status. If digestion is poor or intake is inconsistent, people may fall short on iron or certain B vitamins. That can affect energy and focus. This isn’t a diagnosis, but it’s a practical reminder: the brain runs on fuel, and the gut is the gatekeeper for getting it.
For readers who want a research-focused update on gut-brain links in brain health, here’s a 2025 paper in Scientific Reports: Gut–brain axis and neuropsychiatric health: recent advances.
Inflammation and leaky gut confusion, what we know and what is hype
Inflammation is your body’s normal defense response. A little is helpful. Too much, for too long, can cause symptoms.
Online, you’ll often see “leaky gut” used as a catch-all. The more precise term is intestinal permeability. Your gut lining is meant to be selective, letting nutrients through while keeping many microbes and irritants out. In some diseases, that barrier function can be altered.
The hype problem is when people self-diagnose “leaky gut” as the cause of every symptom and start extreme diets or stacks of supplements. Barrier issues can be real in certain conditions, but the right next step is often basic care and a proper workup, not fear and restriction.
A balanced takeaway: if your gut is irritated, your immune system may be more active, and that can change gut brain communication. But it’s rarely one single cause, and “quick fixes” usually don’t hold up.
Gut feelings are real, but not magic, how your brain interprets gut signals
Your brain doesn’t just receive gut messages, it interprets them.
There’s a simple concept called interoception, which means how your brain senses what’s going on inside your body. Two people can have the same amount of gas or the same gut movement, but one feels mild pressure and the other feels sharp discomfort.
Why? Your brain uses context. Past experiences, current stress level, and sleep quality can all change how the brain reads gut signals. If you’ve had a bad flare before, your brain may get protective and treat small sensations like a bigger threat. That can create a feedback loop: discomfort raises stress, stress raises sensitivity, and the gut feels even worse.
The good news is that loops can be nudged in a better direction. You’re not stuck with one setting.
How to support healthy gut brain communication, simple habits that add up
Most people don’t need a perfect diet or a complicated routine to support the gut-brain axis. They need a few steady habits that lower overall “noise” in the system.
The goal is to help your gut send calmer signals upward, and help your brain send steadier signals downward. That usually means supporting regular meals, better sleep, and a nervous system that gets real recovery time.
If you’ve been chasing answers, start smaller. Consistency beats intensity here. Think in two-week experiments, not lifetime rules.
Food basics for the gut brain axis, fiber, fermented foods, and steady meals
Fiber is one of the most practical tools for gut brain communication because it feeds helpful microbes and supports regular movement. Easy options include beans, lentils, oats, chia, berries, pears, carrots, leafy greens, and potatoes with the skin.
Fermented foods can be helpful for some people, but tolerance varies. If you enjoy them, try small, regular servings like yogurt, kefir, sauerkraut, kimchi, or miso. If they bloat you, that’s useful data, not a failure.
Steady meals matter too. Long gaps can lead to intense hunger, fast eating, and more gut discomfort. A simple plan is three meals, with a snack if you need it, and enough protein and carbs to feel stable.
Hydration supports motility, especially if you’re increasing fiber. Also pay attention to timing. Late-day caffeine can raise anxiety and disrupt sleep, which then feeds back into gut sensitivity. Alcohol can irritate the gut for some people, so moderation helps if you notice a pattern.
Nervous system digestion tools, breathing, movement, sleep, and getting support
If stress affects digestion for you, tools that calm the nervous system are not “extra.” They’re part of digestion care.
Try a few of these and keep it simple:
- Slow breathing before meals: Do 6 slow breaths (in through the nose if you can), and relax your shoulders. This helps shift your body toward rest and digest.
- A short walk after eating: Even 10 minutes can support gut movement and reduce that “stuck” feeling.
- Regular sleep timing: A consistent wake time often helps more than chasing a perfect bedtime.
- Eat a bit slower: Put the fork down once or twice, or take a sip of water. It’s boring advice, but it works.
- Track patterns, not perfection: Keep a short symptom log for two weeks. Note meals, stress level, sleep, and symptoms. People often spot triggers they missed, like rushed lunches, too much coffee, or poor sleep.
If anxiety is high or symptoms are persistent, getting support counts as a health habit. Therapy, stress skills training, and medical care can all reduce the background alarm that keeps the gut-brain axis activated. Changes often take weeks, not days, so give your body time to learn a new baseline.
Conclusion
The gut-brain axis is a two-way loop: the brain can change digestion fast, and the gut can shape mood, energy, and focus through nerves, hormones, immune signals, and microbial byproducts. That’s why anxiety gut symptoms and stress-related digestion shifts are common, and they’re explainable.
Pick one habit to try for the next two weeks, like slow breathing before meals or a short walk after dinner, and see what changes. If symptoms are severe, keep returning, or come with red flags like blood in stool, weight loss, fever, or nighttime pain, talk with a clinician. Your gut and brain are talking, and you can help them communicate with less noise.

Gas S. is a health writer who covers metabolic health, longevity science, and functional physiology. He breaks down research into clear, usable takeaways for long-term health and recovery. His work focuses on how the body works, progress tracking, and changes you can stick with. Every article is reviewed independently for accuracy and readability.
- Medical Disclaimer: This content is for education only. It doesn’t diagnose, treat, or replace medical care from a licensed professional. Read our full Medical Disclaimer here.