If you feel wired but tired, you’re not alone. You might crash hard in the afternoon, then stare at the ceiling at night. Brain fog shows up at the worst times. You crave salty snacks, sugar, or another coffee, even when you know it’ll make sleep harder later.
A lot of people call this “adrenal fatigue.” It’s a relatable phrase, but it can also point you in the wrong direction. In most cases, the clearer lens is HPA Axis Dysfunction, meaning your stress response system is out of sync, not that your adrenal glands have “given up.”
This post explains what’s likely happening inside your body, why it happens, how a clinician might check for common look-alikes, and practical steps that support recovery. No shame, no tough-love lectures, just a calm plan you can start using this week.
What HPA Axis Dysfunction Is, and How Stress Changes Your Body Over Time
Your body has a built-in stress response system. When it works well, it helps you wake up, focus, stabilize blood sugar, and respond to real threats. When it’s been pushed too hard for too long, it can become jumpy, like a smoke alarm that goes off when you make toast.
That’s the heart of HPA Axis Dysfunction. It’s less about “broken” adrenal glands and more about the messaging between the brain, hormones, and nervous system. Stress isn’t only emotional, either. Poor sleep, under-eating, chronic pain, inflammation, and nonstop stimulation can all press the same internal alarm button.
Cortisol is often the headline hormone in this conversation, but it’s not a simple good-or-bad number. Cortisol follows a daily rhythm. For many people, it’s higher in the morning to help you get moving, then it gradually drops so you can wind down at night. A single cortisol test at one time of day may miss the bigger pattern. It’s like taking one photo and trying to understand an entire movie.
When stress becomes chronic, your system may shift resources away from long-term “maintenance” tasks. Digestion can slow down. Immune function can change. Mood can feel flatter, or more reactive. Energy becomes less steady, not because your body is weak, but because it’s trying to keep you safe using the tools it has.
For a clinical view of how the hypothalamic-pituitary-adrenal axis is assessed and interpreted in medicine, see Endotext’s HPA axis testing overview.
Meet your HPA axis, the brain to body stress signal loop
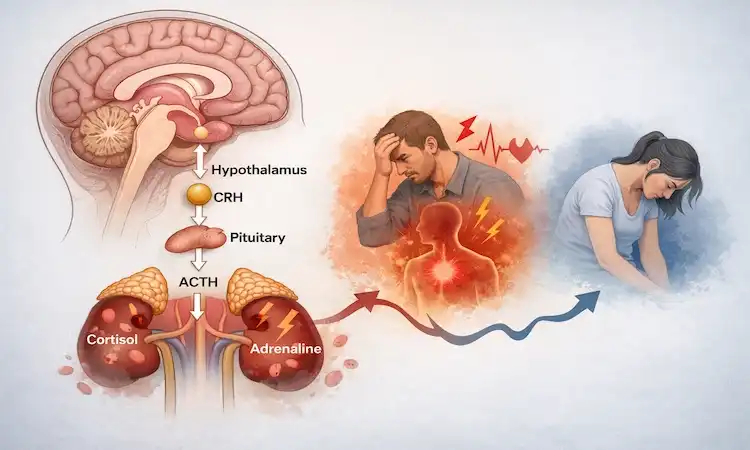
The hypothalamic pituitary adrenal axis is a three-part relay:
- The hypothalamus (in your brain) senses stress and sends a signal.
- The pituitary gland passes that signal along.
- The adrenal glands respond by releasing cortisol and other hormones.
Think of it like a thermostat or volume knob. In a healthy system, it turns up when needed (deadline, illness, hard workout), then turns back down. In HPA Axis Dysfunction, the knob can get stuck too high, too low, or swing around when you least expect it.
Cortisol affects alertness, blood sugar balance, inflammation, and your sleep-wake cycle. That’s why stress problems rarely stay in one “lane.” They show up in energy, mood, gut function, and even how often you catch every bug going around.
Common signs people blame on “adrenal fatigue,” and what they can mean
People often describe a mix of symptoms that don’t seem connected at first. You might notice sleep problems (tired at bedtime, awake at 2:00 a.m.), energy crashes, irritability, anxious buzzing, or a numb, flat mood. Some people get strong cravings (salt, sugar, caffeine), belly weight gain, frequent colds, or slow recovery after workouts. Others notice digestive upset, low motivation, and brain fog that makes simple tasks feel heavy.
These patterns can fit HPA Axis Dysfunction, especially when life has been nonstop. They can also overlap with many other issues, including iron deficiency, thyroid disease, sleep apnea, depression, medication side effects, perimenopause, long COVID, and autoimmune conditions.
Self-diagnosis gets risky fast. The goal isn’t to “claim a label,” it’s to understand your pattern and rule out problems that need direct medical treatment.
What Causes HPA Axis Dysfunction, and Why It Often Shows Up as Burnout
Burnout is rarely one big event. It’s usually the result of repeated stress hits with poor recovery time between them. Your system learns to run hot. Then one day, what used to work (more caffeine, more pushing, more late nights) stops working.
The chronic stress mechanism behind this is pretty simple: your brain keeps detecting demand, so it keeps sending stress signals. If you don’t get enough sleep, food, movement, daylight, or emotional support to balance it out, the “on switch” stays sticky.
Real-life drivers are common and surprisingly ordinary: heavy workloads, caregiving, relationship strain, grief, trauma history, financial pressure, under-eating in the name of “clean” dieting, overtraining, shift work, little morning daylight, alcohol at night to unwind, high caffeine to function, and constant scrolling that never lets your brain fully rest.
Researchers and clinicians describe different burnout recovery stages, but you don’t need strict labels to benefit. What matters is recognizing the pattern: you can feel revved up and exhausted at the same time. You can have a productive morning and then hit a wall after lunch. You can feel worse when you finally stop.
For a research-focused look at recognizing and treating HPA-related patterns in clinical care, you can read An integrative approach to HPA axis dysfunction.
Daily stressors that quietly push the stress response system too hard
Here’s what often “stacks” in the background: sleep debt that becomes normal, blood sugar swings from skipping meals, constant multitasking, relationship tension you keep swallowing, money worry you don’t talk about, chronic pain that never fully lets up, low-grade inflammation, and perfectionism that turns every task into a performance.
Each one might feel manageable alone. Together, they train your stress response system to stay on alert. That’s why someone can have a calm-looking life on paper and still feel like their body is buzzing inside.
A helpful reframe is this: your symptoms may be less about fragility and more about load. When the load stays high long enough, your system adapts, and that adaptation has a cost.
Why symptoms can flip flop, and why you might feel worse when you try to rest
One of the most confusing parts of HPA Axis Dysfunction is the flip flop. Some days you’re tired all day. Other days you’re tired until bedtime, then suddenly awake. Or you can’t relax without feeling guilty, restless, or oddly emotional.
Part of this is nervous system dysregulation. If your body has been relying on stress chemistry to get through the day, slowing down can feel unsafe at first. It’s like stepping off a moving treadmill. Your brain expects motion, so stillness feels wrong, even when you need it.
This also explains why some people get a “post-exertional crash.” Healthy tired is the kind that follows effort and improves with normal rest. Depleted tired is different. It can feel like your battery won’t hold a charge, and overdoing it (hard workouts, late nights, intense social plans) can trigger a longer slump.
Rest isn’t the enemy, but the way you rest matters. Many people do best with gentle, regular downshifts throughout the day, not one giant collapse on the weekend.
How to Check What’s Going On, and When to Get Medical Help
“Adrenal fatigue” isn’t a formal medical diagnosis, but your symptoms are still real, and a clinician can still help you sort out what’s driving them. A good first step is building a simple timeline. When did this start? What changed in work, sleep, training, food, or stress? What makes it better, and what makes it worse?
Track the basics for two weeks: bedtime and wake time, caffeine timing, alcohol, meals, exercise, and symptoms. If you menstruate, note cycle day and any big mood or sleep shifts. This kind of data helps your appointment move faster and reduces guesswork.
Then focus on ruling out common look-alikes. Many “adrenal fatigue” stories turn out to involve iron deficiency, thyroid issues, blood sugar problems, nutrient gaps, sleep disorders, or medication effects. If those are treated, people often feel much better even before they do anything fancy.
If you and your clinician decide to evaluate cortisol, timing matters, and interpretation matters even more. For a clinician-facing overview, see UpToDate’s laboratory assessment of HPA axis function.
Questions to bring to your appointment, plus tests that may rule out look-alikes
Bring a short list of questions. Examples: “What conditions could mimic HPA Axis Dysfunction?” “Are any of my meds affecting sleep or energy?” “Should we screen for anemia or thyroid issues?” “Is my training or diet pattern working against me?”
Common labs your clinician may consider, based on your history, include:
- CBC (anemia, infection clues)
- Ferritin and iron studies (iron stores)
- Thyroid panel (TSH, free T4, sometimes antibodies if indicated)
- B12 and vitamin D
- A1C or fasting glucose (blood sugar patterns)
- CMP (electrolytes, liver and kidney markers)
- Inflammation markers if appropriate for your symptoms
Cortisol testing can be done in different ways (blood, saliva, urine) and at different times of day. The “best” test depends on the question being asked, and results should be read in context, not as a standalone score.
Red flags that should not be brushed off as stress
If any of these are happening, don’t wait it out:
- Fainting or near-fainting
- Unexplained weight loss
- Darkening skin without sun exposure
- Severe vomiting or dehydration
- Chest pain or trouble breathing
- Suicidal thoughts
- Fever that won’t break
- Severe weakness that’s new or worsening
- New neurologic symptoms (confusion, slurred speech, sudden numbness)
Seek urgent care or the ER when appropriate. It’s better to be told “you’re okay” than to miss something serious.
Healing Adrenal Fatigue Naturally: A Realistic Recovery Plan That Supports Your HPA Axis
If you’ve been searching for healing adrenal fatigue naturally, here’s the honest version: recovery usually comes from steady basics, repeated daily, not from one perfect supplement or a strict routine you can’t maintain.
The goal is to make your body feel safe again, using consistent cues: sleep timing, morning light, balanced meals, gentle movement, and planned recovery. Then you slowly reduce the inputs that keep the system revved up (late caffeine, alcohol to sleep, punishing workouts, late-night scrolling).
You don’t need to do everything at once. In fact, doing too much can backfire when your stress response system is already overloaded.
If you want a deeper explanation of how chronic stress affects the HPA axis over time, this paper is a solid reference: Chronic Stress and the HPA Axis.
The basics that move the needle: sleep, light, food, and pacing
Start with a consistent wake time, even on weekends. You’re teaching your body when “daytime” begins. Then get 10 to 20 minutes of outdoor light in the first hour after waking (cloudy light still counts). This supports your circadian rhythm, which supports cortisol rhythm.
At breakfast, aim for protein plus fiber. Think eggs plus berries, Greek yogurt plus chia, tofu scramble with veggies, or a protein smoothie with oats. If you’re prone to crashes, avoid long gaps between meals at first. Steadier blood sugar can reduce that shaky, urgent, snack-hunting feeling that people often blame on “weak adrenals.”
Pacing matters just as much as sleep and food. If your system is depleted, “push through” often triggers a bigger crash later. Try working in small rest breaks before you feel wrecked. Two minutes of slow breathing between meetings can be more helpful than one giant recovery day that never comes.
Reduce stimulants slowly. If you drop caffeine to zero overnight, your fatigue may feel worse and your headaches may spike. A gentle taper tends to be more sustainable.
Nervous system reset tools you can actually stick with
Pick one or two tools you can do daily, even on decent days. Consistency is what retrains the system.
Here are a few options that work well because they’re simple:
- Slow breathing: Inhale through your nose, then exhale a bit longer than you inhale. Do 3 to 5 minutes.
- 10-minute walk after meals: Helps mood, digestion, and blood sugar without stressing your system.
- Light stretching: Two to five minutes, focusing on neck, hips, and calves.
- Relaxing music: One song you associate with calm, headphones on, eyes soft.
- Time in nature: Sit outside or walk near trees, no podcast.
- Social connection: One honest check-in with someone safe.
A simple 2 to 4-week starter plan can look like this:
- Week 1: Set wake time, get morning light, eat a protein-forward breakfast.
- Week 2: Add a 10-minute walk most days, taper caffeine slightly.
- Week 3: Add one nervous system tool daily, set a screen stop time at night.
- Week 4: Keep the basics, then adjust exercise intensity based on recovery.
Track progress in plain terms: sleep quality (not just hours), fewer afternoon crashes, calmer mornings, less “tired but wired” at night, and better tolerance for normal stress.
Supplements can help some people, but they can also complicate things, especially with meds, pregnancy, thyroid disease, anxiety disorders, or high blood pressure. If you want to explore testing-based options, ask a clinician who can personalize it.
Conclusion
If you’ve been feeling wired but tired, foggy, and stuck in a cycle of crashes, your body isn’t failing you. HPA Axis Dysfunction is a practical way to understand how your stress response system can get out of sync after long periods of strain.
The path back usually isn’t dramatic. It’s built on steady inputs, consistent sleep timing, morning light, balanced meals, gentler pacing, and small daily downshifts that teach your nervous system it can stand down.
Start by checking for medical reasons, like results from a cortisol lab, then focus on one change you can stick with. Choose one step today, keep it up for two weeks, and look for small wins like steadier energy and calmer mornings. Your body can adjust over time, and you don’t have to push through by sheer willpower.

Gas S. is a health writer who covers metabolic health, longevity science, and functional physiology. He breaks down research into clear, usable takeaways for long-term health and recovery. His work focuses on how the body works, progress tracking, and changes you can stick with. Every article is reviewed independently for accuracy and readability.
- Medical Disclaimer: This content is for education only. It doesn’t diagnose, treat, or replace medical care from a licensed professional. Read our full Medical Disclaimer here.